Lifestyle Medicine Education: An Answer to Chronic Disease?
Current Situation
The World Health Organisation (WHO) in 2010 found that two-thirds of all death worldwide was due to non-communicable disease, most of which are caused by poor lifestyle choices including tobacco use, unhealthy diet, insufficient physical activity and harmful alcohol intake 1 In April 2015, Margaret Chan, the director of WHO, stated that “non communicable diseases have overtaken infectious diseases as the biggest killers worldwide”.2 It is now estimated that lifestyle-related conditions cost our NHS around £11 billion per year with the combined cost to the NHS and is expected to rise exponentially in the next few decades. 3
It is widely acknowledged that chronic disease has become a major issue for the NHS and for healthcare systems all over the world. The majority of specific disease guidelines include a first stage of management in which giving “lifestyle advice” or encouraging “behaviour change” is the initial recommended step. Despite this being first line management for many chronic conditions it is not an area many practitioners feel confident giving advice in. A recent questionnaire based study in the British Journal of General Practice examined GPs knowledge and confidence in giving advice to patients on physical activity: this revealed that only 20% of responders were broadly aware of national guidelines of physical activity for the population and only 43% were “somewhat” confident of raising the issue of physical activity with a patient 4. Despite the fact that brief advice for physical activity has a number needed to treat of 12, which is 10 times less than smoking, it has been shown that 72% of GPs do not speak to their patients about becoming more active.5,6 This is probably a reflection of the lack of teaching in this area. We are taught how to advise patients on which drugs to use, when to use them, which dose and what effects to see when taking them. It is fair to say many healthcare practitioners do not receive the same level of training on how to give advice to patients on physical activity, diet or other lifestyle behaviours.
What is Lifestyle Medicine?
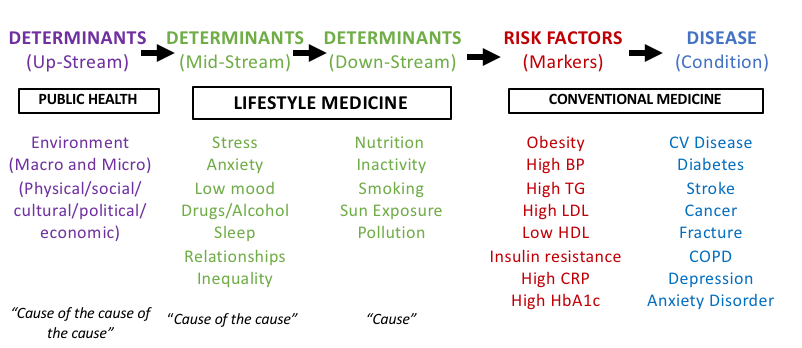
Many of our traditional medical treatments only serve to reduce symptoms or “manage” risk factors of a condition or disease. Lifestyle Medicine aims to actually target the root cause of the problem by looking at upstream determinants of disease that occurred to lead to the medical chronic condition. In attempting to correct the disease-causing process, Lifestyle Medicine has the potential to actually reverse the disease or put the condition into remission. Understanding and acknowledging physical, emotional, environmental and social determinants of disease is essential in order to identify these causes.
The determinants of disease can be categorised into three levels. There are the “Upstream” determinants, such as the environment, which can in turn be divided into the macro- and micro-environment. Politics, economics, social, cultural and physical factors all contribute to environment. Next are the “Mid-stream” determinants which include stress, anxiety, low mood, drugs and alcohol, poor sleep, poor relationships and inequality. Issues in this group commonly lead to poor habits in the next group of determinants of disease called the “Down-stream” determinants. These include nutrition, inactivity, smoking, limited sun exposure and pollution. Upstream determinants of disease are currently managed by public health but the mid-stream and down-stream determinants currently have no formal place in our medical model. It could be strongly argued that this is where Lifestyle Medicine could have an enormous impact.
Lifestyle Medicine involves the use of evidence-based lifestyle therapeutic approaches focusing predominantly on a whole-food and plant-based diet, increasing activity and movement, reducing sedentary behaviour, bettering sleep habits, stress management and relaxation therapy, alcohol moderation and tobacco cessation and other non-drug forms of treatment in order to prevent, treat and reverse the lifestyle-related disease. Although many components of Lifestyle Medicine exist, I find it easiest to look at it within 5 keys areas.
- Activity
- Relaxation
- Sleep
- Nutrition
- Community
Lifestyle Medicine advocates a multidisciplinary, multi-system approach to the chronic disease problem, seeking to involve a varied team who can best educate and inform on these important lifestyle issues. By giving relevant experts a platform to teach we can spread information on ways to improve lifestyle and health. For example, learning about nutrition from nutrition experts, learning about relaxing from meditation experts and sleep from sleep experts.
Why Lifestyle Medicine?
The majority of healthcare professionals entered the profession as they wanted to help their patients become and stay healthy with the main outcome that they go on to live happier lives. Unfortunately the current medical model often does not push towards these desirable outcomes. There are many reasons for this. It could be argued that the focus on symptoms and markers of disease is so strong that the “wood is not seen for the trees” and the root causes are ignored. Time pressures can be to blame as well as the multiple targets continually set for healthcare professionals leaving little time for addressing underlying causes.
Regardless of the reasoning there is no doubt that the current medical model is struggling. The prevalence of chronic disease continues to rise, accompanied by an unsustainable financial cost to the NHS. Alongside this, levels of career dissatisfaction within the medical profession continue to rise, pushing increasing numbers of healthcare professionals into early retirement, “burn out” or career change.
A different approach is needed: one that focuses on addressing the root cause of the problem; one that inspires practitioners as they are able to prevent, reverse and cure chronic disease. No medical professional gets much satisfaction from starting a drug medication and reducing a HbA1c from 64 to 58. However, think of the level of satisfaction and pride associated with having the tools to help a patient reverse their condition and in doing so improve energy levels, happiness and general vastly improve their quality of life.
It is important to recognise that consultation techniques are key to helping patients make changes in their lifestyle. Motivational interviewing methods are essential for assessing motivation to change and confidence in making that change. It can also identify concerns, fears and barriers, which are important to address before attempting to make a change. By understanding the evidence around Lifestyle Medicine and by employing motivational interviewing techniques, healthcare practitioners may utilise Lifestyle Medicine to revolutionise patient care. Lifestyle Medicine may also have the power to revitalise a work force whose deep desire is still to care holistically for patients and allow them to live healthier and happier lives.
Obstacles to Lifestyle Medicine?
The only way in which healthcare professionals will gain confidence in Lifestyle Medicine is if they are taught the information regarding the evidence base of the subject as well as the tools to allow them to help patients make lifestyle changes such as motivational interviewing. Unfortunately, there is very little teaching on lifestyle medicine or behaviour change in undergraduate or post-graduate education. Without the knowledge and the tools, it is very difficult to implement Lifestyle Medicine. This may explain to some extent the limited success most practitioners experience and why many are demoralised by the concept of trying to encourage their patients to change their behaviours.
Teaching to Medical Students
In order to the issue that healthcare practitioners do not know how best to use Lifestyle Medicine, we need to look at the beginnings of their careers. If healthcare professionals do not have Lifestyle Medicine integrated into their practice from the start of their training then it makes it difficult to change habits later on in their careers. This supports the idea of integrating Lifestyle Medicine teaching and motivational interviewing into the undergraduate curriculum for all healthcare professionals.
I have been involved in implementing a “Prevention Medicine” Day at Bristol University. This day is a central study day for 3rd year medical students. It originally started as a ½ day teaching on nutrition but has developed over the last four years into full day teaching on Lifestyle Medicine. The day involves a mixture of lectures, workshops and role plays as well as practical demonstrations in which food is prepared by cooking experts. The idea of Lifestyle Medicine is introduced, as well as specific teaching on physical activity, diet, motivational interviewing and a brief look at the environmental aspect of the issues associated with Lifestyle Medicine such as the food environment and the cost of food. The day involves one tutor for every 12 students, with around 200 students attending in total. The tutors are all junior doctors or full time doctors with a keen interest in lifestyle medicine.
These “Prevention Medicine” days have generated a great interest in Lifestyle Medicine from both students and tutors who have taken part in the day and has led to the development of student selected studies at Bristol University that focus on components of Lifestyle Medicine such as diet. The day is currently being developed into a set program with support from the British Society of Lifestyle Medicine which can be repeated at other medical schools to spread the message further of Lifestyle Medicine to other medical schools in the country.
Although this is just a start, the event will hopefully spark more enthusiasm from doctors and students at these various medical schools to drive Lifestyle Medicine into the undergraduate curriculums in all medical schools. Once this has been achieved then hopefully this sort of teaching will spread to other healthcare professional degrees and courses.
Teaching to GPs
Lifestyle Medicine is useful to all practitioners. One obvious group of healthcare practitioners who can have significant impact are those in primary care. Although the idea of a family doctor is not what it used to be, there is still continuity with a GP that one does not get with many other healthcare professionals. For this reason, I was keen to target GP teaching sessions. I was lucky enough to work for Public Health in Wiltshire during my GP training and in that time I taught on the subject of physical activity to over 15 GP practices as well as to regional teaching groups of GPs in Bath and Wiltshire.
As part of my role as the Leadership Scholar for Severn Deanery in my last year as a trainee I decided to set up a conference on several aspects of Lifestyle Medicine for GPs and GP trainees. I was fortunate to get several very well respected speakers to talk including Dr William Bird, Dr Ali Khavandi, Dr Rupy Aujla and Dr Zoe Williams. This conference included information on several aspects of Lifestyle Medicine, including physical activity work outs with a local personal trainer, food demonstration by Dr Rupy Aujla and a panel discussion with all the guest speakers and the opportunity for delegates to ask questions around Lifestyle Medicine. It also included specific teaching on motivational interviewing by Dr Tim Anstiss, the founder of the Academy for Health Coaching, who taught specific methods to help practitioners help patients change their habits. The day was a sell out and the feedback proved delegates’ enthusiasm for the subject. The conference was put forward for the RCGP Vibrant Faculty Award for South West.
Due to the success of this event, funding was given for a second Lifestyle Medicine conference in Bristol which focused on practitioner health. This conference involved lots of practical workshops including several different types of workouts from yoga to high intensity interval training to jogging to a gentle walk. Separate sessions on meditation and mindfulness were taught by a mindfulness expert from London called Michael James Wong and gave delegates the chance to meditate and zone out from their busy schedules. Many admitted they had not practiced this for many years and couldn’t believe how relaxing and enjoyable they found it.
Workshops were also organised specifically looking at diet myths, looking at the science behind low carb diets and what diet is best implicated for heart health. The day received some very positive feedback and there are already plans in place for another conference to hopefully reach more GPs and practitioners in primary care and beyond.
What’s next?
I feel Lifestyle Medicine is a game changer as it has the chance to transform patients lives but also transform practitioners work to become more enjoyable and fulfilling. One thing that was clear during all these teaching events and conferences was the vast enthusiasm for this subject. Both students and health care practitioners that have attended the different sessions have all given formal and formative feedback expressing their delight at how they enjoyed learning more about this subject and they wished for more training of similar nature.
Thanks to the British Society of Lifestyle Medicine, it appears that several more of these events will be starting to appear imminently. The annual British Society of Lifestyle Medicine Conference is happening this summer and already has a fantastic line up of speakers. The society is also running the International Board of Lifestyle Medicine diploma in August 2021.
If you are interested in this subject, learning more or want to get involved with the British Society of Lifestyle Medicine then please do get in touch with us directly via the website.
References
- WHO Global Status Report on Noncommunicable Diseases 2010 - http://www.who.int/nmh/publications/ncd_report_full_en.pdf
- WHO Director-General addresses the place of noncommuicable diseases in strategies and agendas - http://www.who.int/dg/speeches/2015/ncd-development-cooperation/en/
- BBC Health – Illnesses associated with lifestyle cost the NHS £11bn - http://www.bbc.co.uk/news/health-37451773
- Chatterjee R, Chapman T, Brannan M and Varney J. GPs’ knowledge, use and confidence in national physical activity and health guidelines and tools: a questionnaire-based survey of general practice in England. Br J Gen Pract 2017;67 (663):e668-e675
- Brooks J. Promoting physical activity: the general practice agenda. Br J Gen Pract 2016 Sep;66(650): 454-455
- Macmillan Cancer Support. Move More – Physical Activity the underrated ‘wonder drug’.